Real growth. Real rewards.
Lasting results, powered by AI,
our team of licensed clinicians, educators, kids and YOU!
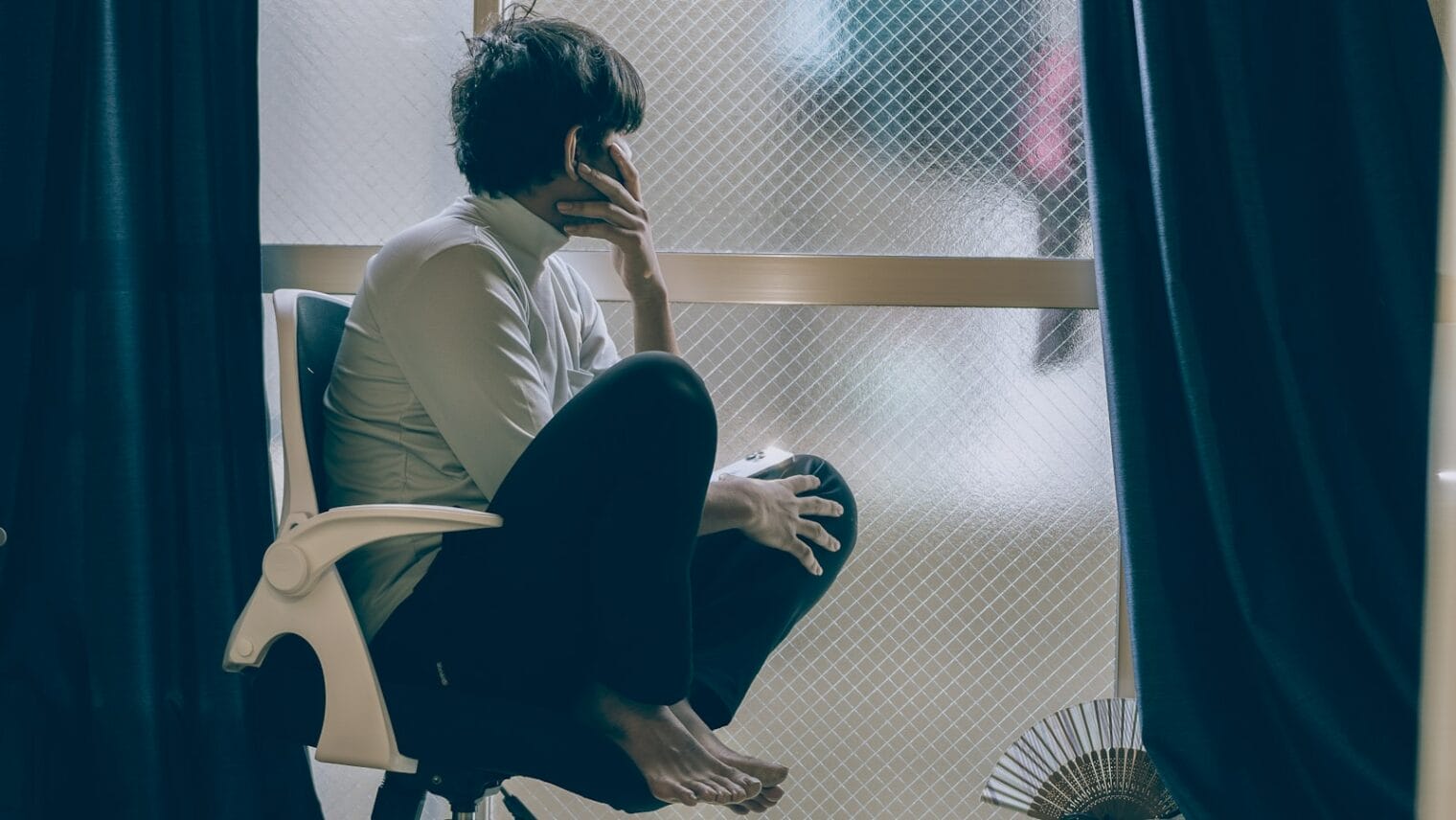
Families’ wellness is interconnected, and being well goes beyond physical health. curaJOY provides effective and continuous wellness support for diverse families, combining behavioral healthcare, education and AI to foster growth and genuine relationships.
Solid Science
Digitized clinical protocols that work, including Somatic Psychotherapy and Acceptance Commitment Therapy, with support from clinicians and partnerships with leading universities.
Whole Family
We not only develop social emotional skill but guide you through enough real-life practice for lasting change, healthier relationships and family environments.
Ultimate Control
Own your data, and connect with various service providers and educators, while keeping all educational and behavioral health data in one place.
Have Fun
Doing good doesn’t have to be boring! Nothing works if you can’t stick to it. We use 3D animation, social media, chats and real-world rewards to engage and retain users.
THE MISSING LINK IN WELLNESS
Personalized and On-Demand Coaching and Behavioral Health Support
curaJOY provides gamified, inclusive, and on-demand behavioral health platforms using emerging technologies like AI with clinician supervision to reinforce positive habits in kids and families. Traditional therapy can cost up to $200/hour, and immediate, on-demand care is scarce.
Healthcare
👍 Save time and money. Easily ensure compliance.
Grow your capacity with automation.
Schools
Deliver IEP and Social Emotional Learning without overworking teachers.
Culturally-inclusive services for diverse student bodies.
Families
Skip the wait lists and treatments that don’t work
On-demand, no scheduling
International
Can’t find ABA or trauma-informed care in your country?
Get the best whole-person wellness support from the US.
Think more positively
Boost self-esteem
Decrease anxiety and stress
Live better
Better relationships
Excel academically
Lessen harmful behaviors
Improve social skills
Working to solve major social and mental health related problems jointly with our communities and cross-sector collaborations.
We improve family emotional wellness globally through integrating latest advancements from tech, behavioral healthcare, education and gaming. This is a purpose too important to be for-profit.